Castelletti Francesca: Pediatrics department, Ospedale dei Bambini Vittore Buzzi, Università degli studi di Milano (Italy)
R. Grandinetti: Pediatrics department, Ospedale dei Bambini P. Barilla, Università degli studi di Parma (Italia)
Interconnectedness of climate change and air pollution
Climate change and air pollution are closely interlinked phenomena that amplify each other, with significant consequences for respiratory infections and
diseases. Together, they represent a growing threat to global health. The combined impact of these two factors is one of the most urgent health challenges worldwide: climate change is set to increase the frequency and intensity of extreme weather events, which in turn contribute to higher levels of air pollutants, thus aggravating respiratory diseases. In addition, continued economic and population growth in many regions of the world will lead to a further increase in pollutant emissions, resulting in an increase in the global burden of respiratory diseases. This scenario particularly affects the most vulnerable segments of the population, such as children, the elderly, and people with pre-existing respiratory conditions. 
The burden of respiratory diseases related to air pollution in vulnerable populations
Children’s respiratory systems, in particular, are more sensitive to the effects of air pollution than those of adults.
Early exposure to environmental pollutants is associated with an increased risk of developing asthma and chronic
obstructive pulmonary disease (COPD), with long-term consequences for respiratory health. Air pollution significantly exacerbates numerous respiratory diseases, including infectious diseases, asthma, allergic rhinitis, chronic obstructive pulmonary disease (COPD), and lung cancer.
- Childhood asthma: Climate change, combined with air pollution, can promote the development of asthma in children. Studies conducted on European paediatric populations have shown that, during heat waves, the interaction between particulate matter (PM) and asthma symptoms becomes more pronounced. These extreme weather events seem to intensify the harmful effects of pollution on respiratory health. Asthma is in fact the respiratory disease most closely linked to pollution in children, due to their still-developing immune systems and greater exposure to pollutants, which increase the risk of exacerbations.
- COPD: Chronic obstructive pulmonary disease, an adult disease that generally develops after the age of 40, is a growing public health problem, exacerbated by both climate change and air pollution. A systematic review with meta-analysis of eight studies found a 1.12-fold increase in the risk of mortality from COPD for every 10 μg/m3 increase in PM2.5. In addition, air pollution can worsen the severity of emphysema in patients with COPD.
- Allergic rhinitis: This globally prevalent condition is closely linked to exposure to air pollutants. The impact is particularly evident in developing countries, where pollution levels are often higher and healthcare systems are less well equipped.
- Upper respiratory tract infections: Exposure to particulate matter (PM), particularly in children and adolescents, is associated with an increase in upper respiratory tract infections, with potentially lasting effects on lung development.
- Lung cancer: Outdoor air pollution, especially in its fine particulate matter (PM2.5 and PM10) components, has been officially classified as carcinogenic to humans by the International Agency for Research on Cancer (IARC), underscoring the seriousness of prolonged exposure to these substances.
The negative effects of air pollution on respiratory health can be amplified by climate change and an increase in extreme weather events. In this context, it is essential to identify the environmental factors associated with respiratory diseases, particularly in order to protect the most vulnerable populations. These factors contribute to lung inflammation, oxidative stress, and impaired immune function in the respiratory system.
Public health and the environment: strategies for protecting respiratory health
To mitigate the combined impact of climate change and air pollution on respiratory health, targeted public health strategies are needed, including:
- Reducing greenhouse gas emissions to slow global warming and limit its health impacts;
- Mitigating the frequency and intensity of extreme weather events through adaptive and resilient climate policies;
- Improving air quality through regulatory and technological innovations that can help reduce the incidence and morbidity of respiratory diseases;
- Implementing inclusive health and social policies aimed at ensuring equitable access to medical care and strengthening support systems for communities most exposed to the adverse effects of pollution and climate change.
In summary, there is an urgent need to promote ongoing research, effective policies, and targeted public health interventions to address the complex challenges posed by climate change, air pollution, and their impact on respiratory health. Future projections indicate that these factors will significantly influence the incidence of respiratory diseases, especially among the most vulnerable populations. Concrete, coordinated, and evidence-based actions can help protect respiratory health and improve overall public health outcomes.
Artificial intelligence platform in healthcare systems
In this regard, a study conducted at the Sabarà Children’s Hospital (São Paulo) examined how hospitals and healthcare systems can benefit from artificial intelligence (AI) and big data by combining clinical information with external sources. In particular, machine learning, a branch of AI, uses algorithms trained on large data sets to predict emergency room visits and hospital admissions for respiratory diseases, using both clinical and environmental data. The authors emphasize the value of the combined approach: the predictive component (AI) is complemented by traditional epidemiological models, which quantify in an interpretable way the associations between environmental exposures and paediatric respiratory health. These algorithms can distinguish, for example, whether a child who arrives at the emergency room is likely to be discharged or will require hospitalization. This predictive capability is particularly useful for improving hospital planning and resource allocation, especially in contexts exposed to environmental vulnerabilities.
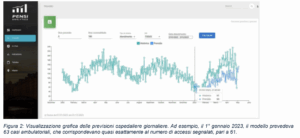 In conclusion, one of the most promising tools for addressing the challenges posed by climate change is the
In conclusion, one of the most promising tools for addressing the challenges posed by climate change is the
development of integrated platforms that combine clinical and environmental databases within a big data
infrastructure, leveraging the potential of artificial intelligence for information analysis and processing.
Bibliography
– Tran, H. M., Tsai, F. J., Lee, Y. L., Chang, J. H., Chang, L. T., Chang, T. Y., … & Chuang, H. C. (2023). The impact of air pollution on respiratory diseases in an era of climate change: A review of the current evidence. Science of the Total Environment, 898, 166340.
– Cabral-Miranda, W., Beloni, C., Lora, F., Afonso, R., Araújo, T., & Fernandes, F. (2025). Artificial intelligence
platform to predict children’s hospital care for respiratory disease using clinical, pollution, and climatic
factors. Journal of Global Health, 15, 04207.
No metadata found.



