An Israeli study conducted on patients with bronchopulmonary dysplasia (BPD) evaluated the usefulness of flexible bronchoscopy (FB) in obtaining information on the prevalence of airway anomalies.
Definition and Incidence of BPD
Bronchopulmonary dysplasia (BPD) represents a significant challenge in pediatric pulmonology, as it is the leading cause of late morbidity in preterm infants. Despite improvements in perinatal care, the overall incidence of BPD has remained unchanged in recent decades due to increased survival rates of extremely premature infants. Currently, in the United States, it affects approximately 10,000 infants annually. The incidence of BPD in infants born before 28 weeks of gestational age (GA) is estimated between 48% and 68%, with an inverse relationship to GA.
Study Type and Hospital Setting: Sample Details and Control Group
A retrospective case-control study was published in the European Journal of Pediatrics, conducted on BPD patients who underwent FB at a tertiary-level Israeli hospital (Soroka University Medical Center) between 2013 and 2023. BPD patients (50 children) were matched (1:3) to a reference group (150 children) based on age (mean age 1.26 ± 0.9 years), sex (58% male), and ethnicity, all of whom also underwent FB.
Bronchoscopy Procedure and Instrumentation
All bronchoscopies were performed under the same sedation conditions, by the same endoscopist staff, and with the same equipment (Olympus pediatric bronchoscopes with external diameters of 2.8 or 3.6 mm).
Statistical Analysis and Data Interpretation
Descriptive statistical analyses were conducted to evaluate various characteristics of the study population. Continuous variables with a normal distribution are presented as mean ± standard deviation (SD), while continuous variables with a non-normal distribution or ordinal variables are presented as median and interquartile range (IQR). Categorical variables are presented as frequency and percentages.
Association Between Bronchoscopic Findings and BPD Diagnosis
To determine the association between bronchoscopy findings and the presence of BPD, a univariate logistic regression was performed. This analysis provided odds ratios (OR) for each bronchoscopy finding, serving as a measure of the strength of association with BPD. The significance level was set at P<0.05 (two-tailed).
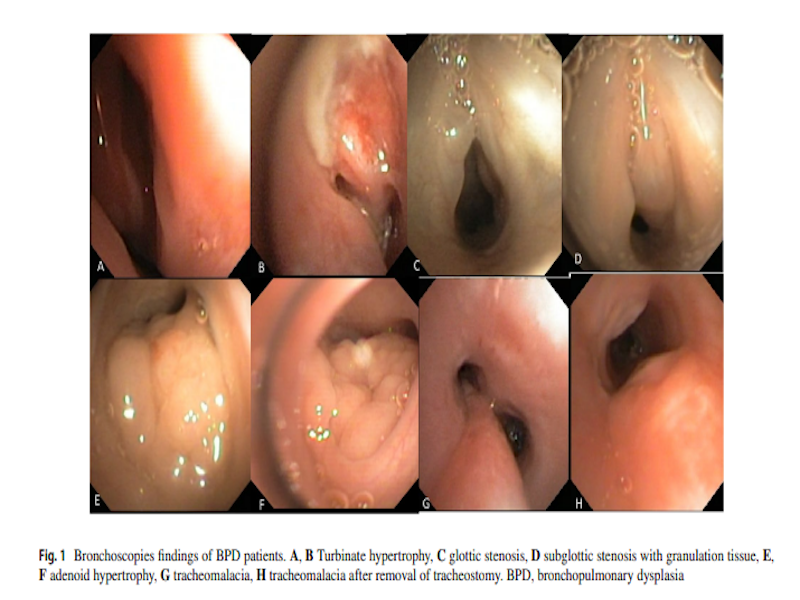
Study Results and Limitations: Main Anomalies Detected in BPD Patients
As expected, anatomical anomalies (primarily of the upper airways) were significantly more common in the BPD group compared to the reference group, with a significant increase in turbinate hypertrophy, adenoidal hypertrophy, and especially subglottic stenosis and tracheomalacia.
Complications During and After the Procedure
Beyond the findings, the authors focused on complications during and after the procedure. Episodes of prolonged desaturation (OR: 3.89, P = 0.013), indicative of reduced pulmonary reserve and airway vulnerability during the procedure, the need for intubation at the end of the procedure (present in the BPD group but P not evaluable as there were no intubation episodes in the control group), and admission to intensive care post-endoscopy (OR: 16.6, P = 0.011) were more frequent in the BPD group compared to the reference group.
Criticisms and Limitations: Sample Size and Comorbidities
Although the authors report that there are apparently no other case-control studies in the literature comparing endoscopic findings between BPD patients and patients without chronic respiratory diseases, this study has at least two limitations. Firstly, the small sample size of 50 BPD patients undergoing FB is noteworthy; however, most results were statistically significant, supporting the findings and potentially highlighting underdiagnosis. Secondly, given the higher prevalence of other comorbidities within the BPD group, it is plausible that some of the observed differences between the groups could be attributed to factors beyond the BPD condition.
Conclusions and Clinical Implications
The authors conclude that, although the study revealed a high prevalence of structural anomalies leading to airway obstruction in BPD patients, the use of an invasive procedure like flexible bronchoscopy requires careful evaluation, adequate expertise of the operating center, and the need for intensive support in case of post-procedural complications in this vulnerable population.
Bibliography
Noa Shemesh Gilboa, Micha Aviram, Aviv Goldbart, Guy Hazan, Noga Arwas, Itai Hazan, Daniel Yafit, Sergey Tsaregorodtsev, Inbal Golan-Tripto. Flexible bronchoscopy in preterm infants with bronchopulmonary dysplasia: findings and complications in a matched control study. Eur J Pediatr. 2024 Nov;183(11):4837-4845. doi: 10.1007/s00431-024-05750-w. Epub 2024 Sep 9.
FAQ on the Utility of Flexible Bronchoscopy (FB) in Assessing Airway Anomalies
-
What is the role of flexible bronchoscopy in managing bronchopulmonary dysplasia in preterm infants?
Flexible bronchoscopy (FB) has been used to explore the incidence of airway anomalies in preterm infants with BPD. This diagnostic tool allows for visual assessment of airway structures, highlighting structural anomalies that may contribute to respiratory obstruction and worsen the clinical picture of BPD.
-
What airway anomalies were identified in neonates with BPD through bronchoscopy?
The study found a higher prevalence of anatomical anomalies in neonates with BPD compared to the control group. The main anomalies were turbinate and adenoidal hypertrophy, subglottic stenosis, and tracheomalacia. These alterations contribute to airflow limitation and increase airway vulnerability.
-
What were the most frequent complications associated with bronchoscopy in BPD patients?
Complications included episodes of prolonged desaturation (indicative of reduced pulmonary reserve), need for post-procedure intubation, and admission to intensive care post-endoscopy. These complications underscore the vulnerability of BPD patients during invasive procedures like bronchoscopy.
-
What are the limitations of the study, and how might they influence the results?
The study had two main limitations: a relatively small sample size (50 BPD patients) and the presence of comorbidities within the BPD group. These factors may limit the generalizability of the results and suggest the need for larger studies to confirm the observed findings.
-
What clinical implications emerge from the study for treating BPD in preterm infants?
The study’s results indicate that flexible bronchoscopy can be a useful tool for identifying airway anomalies in neonates with BPD. However, due to the observed complications, bronchoscopy should be reserved for carefully selected cases and conducted in centers with specialized expertise and availability of intensive support.
No metadata found.